
For those exploring advanced healthcare roles, it’s common to compare nurse practitioners (NPs) and physician assistants (PAs). Both NPs and PAs are licensed healthcare professionals who diagnose conditions, prescribe medications and provide essential patient care.
However, their educational backgrounds, clinical training models and levels of practice independence differ in key ways. This guide breaks down everything prospective students need to know, including education requirements, scope of practice, professional autonomy, salary expectations and long-term career paths.
While both roles offer meaningful work and strong job outlooks, aspiring NPs may find added benefits — especially those interested in specializing in patient populations or working independently. Programs like the online Master of Science in Nursing (MSN) – Family Nurse Practitioner (FNP) program from Northern Kentucky University (NKU) prepare students for these opportunities with online coursework and clinical placement support.
Education: NP vs. PA
The educational paths for nurse practitioners and physician assistants share some similarities. However, they diverge in structure, focus and clinical training models. To become a nurse practitioner, students must first become a registered nurse, usually by completing a Bachelor of Science in Nursing (BSN).
From there, they pursue an MSN or a Doctor of Nursing Practice (DNP). NP programs are built on the nursing model, which focuses on patient-centered care and often includes specialization by population, such as family medicine, women’s health or psychiatric mental health.
Physician assistants typically hold a bachelor’s degree in a science-related field before entering an accredited physician assistant program at the master’s level. These programs follow the medical model, which is similar to physician training and emphasizes disease pathology, treatment plans and generalist care.
Both tracks require intensive clinical training. NP students complete clinical hours with a focus on their chosen population group, while PA students complete clinical rotations in areas such as emergency medicine, family practice and surgery. Certification is also distinct; NPs take board exams relevant to their specialization, while PAs must pass the Physician Assistant National Certifying Exam (PANCE) administered by the National Commission on Certification of Physician Assistants (NCCPA).
Common prerequisites for both programs include hands-on clinical hours, prior experience in patient care and meeting licensure and educational standards set by state and national boards. According to the U.S. Bureau of Labor Statistics (BLS), both physician assistant and nurse practitioner roles are in high demand and require advanced coursework and certification.
Scope of Practice Differences
Nurse practitioners and physician assistants both provide critical care across a range of clinical settings. However, their scope of practice and legal authority differ based on education, training and state regulations.
Nurse practitioners (NPs) receive training to provide comprehensive care. Their responsibilities include diagnosing conditions, prescribing medications, developing treatment plans, and offering both primary and specialized care. NPs can choose to specialize in patient populations such as family health, psychiatric mental health, pediatrics, women’s health and gerontology, tailoring their practice to serve specific community needs.
Physician assistants (PAs) also diagnose and treat illnesses, write prescriptions and manage patient care. However, their practice is typically under the supervision of a physician, though the degree of oversight varies by state. Unlike NPs, PAs are trained as generalists, allowing them to work across various specialties such as emergency medicine or outpatient surgery throughout their careers.
Both professions are integral to preventative care and are commonly found in outpatient settings, helping increase healthcare access and reduce system strain. State laws significantly shape what each role is permitted to do independently.
|
NP vs. PA Scope of Practice |
||
| Category | Nurse Practitioner (NP) |
Physician Assistant (PA) |
| Diagnosing patients | Yes | Yes |
| Prescribing medications | Yes | Yes |
| Treatment planning | Yes | Yes |
| Independence | May practice independently in many states | Generally requires supervision of a physician |
| Specialization options | Family, psychiatric mental health, pediatrics, women’s health, gerontology | Trained as generalists; can work across specialties |
| Typical settings | Primary care, outpatient clinics, specialty practices | Hospitals, outpatient clinics, emergency departments |
| Model of care | Nursing model — patient-centered, population-focused | Medical model — disease-centered, physician-style |
Independence and Autonomy
Nurse practitioners often have greater independence, which makes the role more appealing to those seeking a more self-directed practice. Many states recognize NPs as advanced practice registered nurses (APRNs). They can act as primary care providers without needing a physician’s supervision.
This independence is especially important in underserved areas where access to doctors may be low. NPs in outpatient settings often lead care teams and make decisions on their own based on their training and specialization.
PAs, by contrast, generally operate with collaborative or supervisory agreements in place, as required by most state laws. While they can switch specialties and provide broad medical support, their scope is closely tied to a physician’s oversight and the practice setting’s guidelines. For up-to-date information on where NPs can practice independently, consult the AANP’s state practice environment map.
NP vs. PA Salary
Both nurse practitioners and physician assistants enjoy competitive salaries. Earnings vary based on factors such as location, specialization and years of experience. According to the U.S. Bureau of Labor Statistics (2024), the median salary for nurse practitioners is $132,050, while physician assistants earn a median salary of $133,260.
Factors that influence income include whether the professional works full-time, their chosen patient population and geographic location. NPs often work in high-demand areas like preventative care, which continue to see growing need due to national healthcare shortages. Both roles offer strong career outlooks, with increasing opportunities for leadership and advancement as the healthcare system evolves.
Career Outlook and Job Growth
The career outlook for both nurse practitioners and physician assistants is exceptionally strong, driven by ongoing demand for qualified healthcare providers in various clinical settings. BLS projects that the employment of nurse practitioners will grow by 35% from 2024 to 2034, while expectations for growth in the employment of physician assistant roles are 20% during the same period, both significantly faster than the national average for all occupations.
The rising need for preventative care, chronic condition management and expanded access to care in underserved areas largely fuels this growth. Opportunities are especially abundant in primary care, acute care, nursing homes, outpatient clinics and increasingly, telehealth. As the population ages and access to physicians remains limited in many regions, both NPs and PAs will continue to play essential roles in general medicine and family practice.
Choosing Between NP and PA
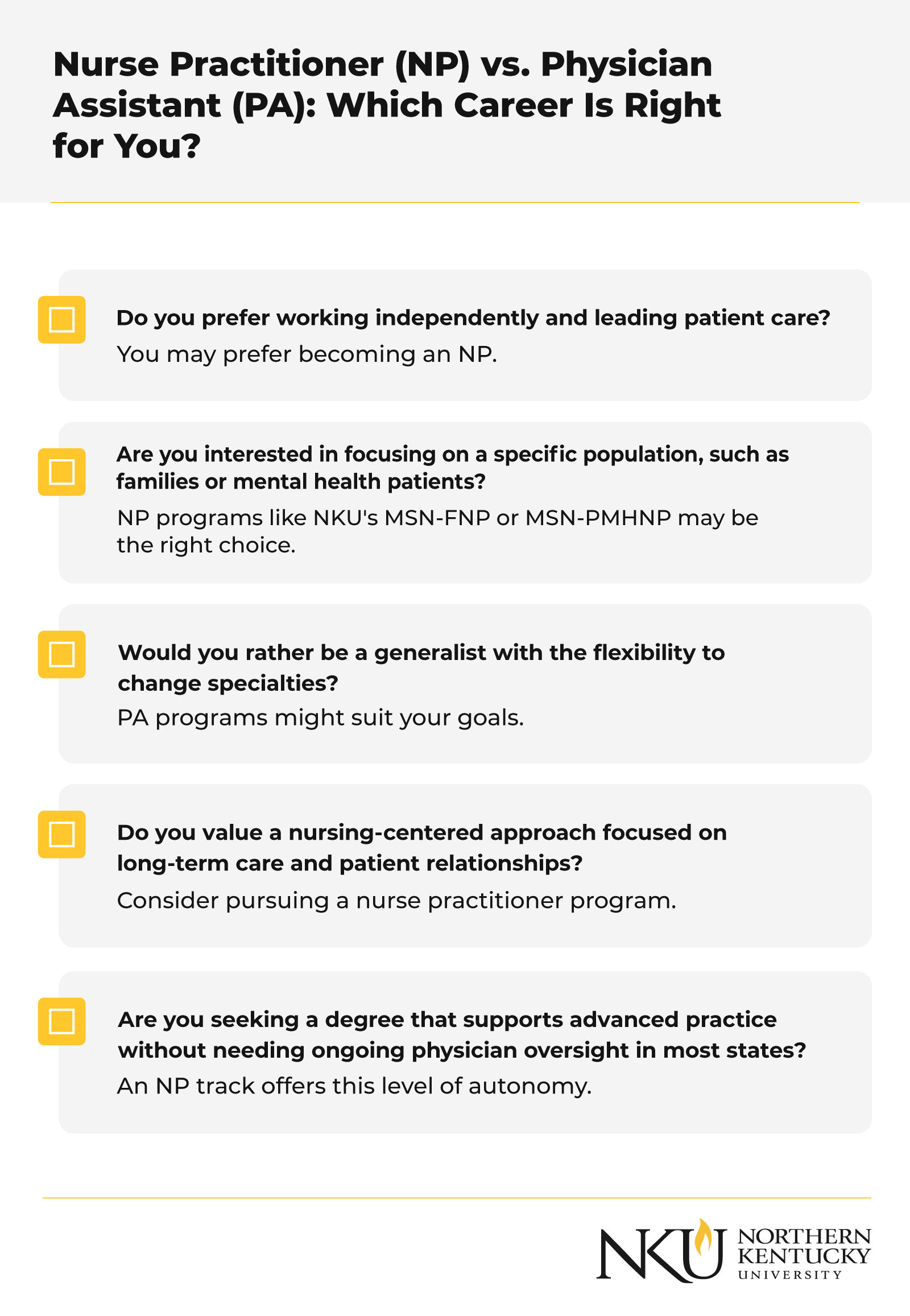
Choosing between becoming a nurse practitioner or a physician assistant depends on your educational background, desired career flexibility and long-term goals. If you’re drawn to independent practice, working closely with defined patient populations and tailoring care through a nursing-focused model, then the NP path may be a better fit.
Specialties like pediatrics, psychiatric mental health and gerontology offer NPs the opportunity to make a meaningful impact while maintaining autonomy and leadership in their field. Use the checklist below to assess which path aligns with your goals:
Whichever path you choose, both careers offer rewarding, high-growth opportunities. For those leaning toward NP, NKU’s online MSN program provides a strong foundation to advance your career in healthcare.
NKU’s MSN FNP Program for Nurse Practitioners
Nurse practitioners and physician assistants share the goal of delivering excellent patient care, but they differ in several meaningful ways. NPs typically follow a nursing-based education path, specialize in distinct patient populations and can often practice independently.
In contrast, PAs follow the medical model, are trained as generalists, and usually work under the supervision of physicians. These differences affect their scope of practice, degree of autonomy and long-term career paths.
Both roles offer competitive median salaries and growing opportunities within the healthcare system. For those leaning toward nursing, a career as an NP offers the chance to provide focused, patient-centered care with greater independence. NKU‘s online MSN – FNP program prepares future healthcare professionals for leadership roles in a flexible format built around your life and goals.
FAQ
The following FAQs address common questions about becoming an NP or PA, covering education, autonomy, practice scope, compensation and more. Keep in mind that answers reflect national standards and trends; specifics can vary based on state regulations and employer policies.
Is a physician assistant higher than a nurse practitioner?
Not necessarily. There’s no formal hierarchy. Nurse practitioners and physician assistants have different training models and scopes of practice. NPs are advanced practice registered nurses (APRNs) and may practice independently in many states, particularly in primary care. PAs typically work under the supervision of a physician, though their clinical authority can still be substantial. The key differences depend on state laws, the setting and the role structure.
What can a PA do that an NP cannot?
PAs are trained under the medical model and are considered generalists, which means they can shift specialties (e.g., from emergency medicine to surgery) without earning a new degree. NPs generally specialize by patient population, such as family medicine or psychiatric mental health, and may need post-graduate training or certification to switch specialties.
Is it harder to become an NP or a PA?
Both paths are academically rigorous and require extensive clinical hours and graduate-level classes. To become an NP, most students first earn a BSN, then pursue an MSN or DNP, along with licensure and board certification.
To become a PA, students need to complete a master’s degree from an accredited PA program and pass the PANCE. The challenge often depends on your background. Nurses may find the NP route more familiar, while others may prefer the PA structure better.
What is a nurse practitioner’s scope of practice?
NPs can diagnose conditions, order and interpret diagnostic tests, prescribe medications, and create treatment plans. Many states allow NPs full practice authority, meaning they can provide care without physician supervision. Others require collaborative agreements. You can view each state’s policy through the AANP state practice environment map.
What degree do you need to become a registered nurse?
To become a registered nurse (RN), you need either an Associate Degree in Nursing (ADN) or a BSN. After graduation, passing the NCLEX-RN exam is required for licensure. Employers often prefer the BSN, which is a prerequisite for most nurse practitioner programs.
Is healthcare a good career path?
Yes. Healthcare continues to show strong job growth and offers a wide range of roles across clinical and non-clinical settings. BLS projects 35% growth for NPs and 20% for PAs from 2024 to 2034, making both occupations among the fastest-growing.