
Healthcare organizations across the U.S. are preparing for an important generational shift as many experienced baby boomers approach retirement. This transition is encouraging leaders to modernize systems, strengthen support for frontline workers and find new ways to build resilient, skilled teams. To better understand worker sentiment during this period of change, a national questionnaire was conducted among 300 healthcare workers on behalf of Northern Kentucky University. They shared insights about staffing, reskilling, technology and long-term career outlook.
This research aimed to understand how workforce changes are impacting employees and to identify opportunities to enhance stability and growth. Current healthcare workers have concerns about staffing and workload, but they also expressed a strong motivation to pursue new skills, adopt helpful technologies and remain committed to the field. Their responses point to a healthcare workforce that is ready to adapt and move forward with confidence.
Key Takeaways
- Over half of healthcare workers (51%) say upcoming retirements on their team will increase their workload, and nearly as many (49%) warn they’ll lose critical team knowledge as older staff exit.
- Over four in five healthcare workers (85%) believe the workforce is becoming increasingly strained.
- Nearly two in five healthcare workers (38%) feel confident their employer is addressing staffing shortages.
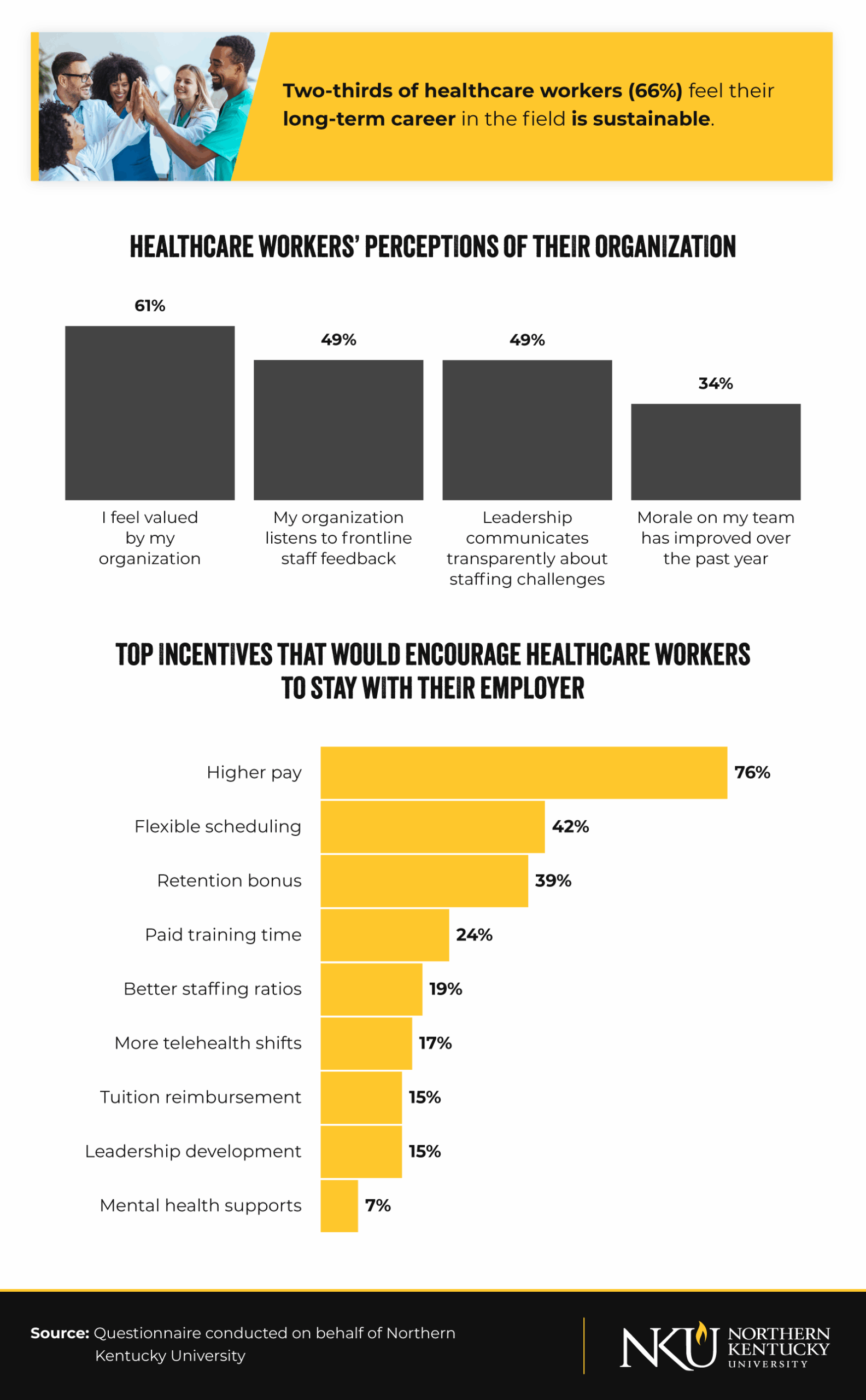
- Two-thirds of healthcare workers (66%) feel their long-term career in the field is sustainable.
- Over three in five healthcare workers (63%) are interested in reskilling or upskilling within the next two years.
How Retirements and Workload Trends Are Shaping Today’s Healthcare Teams
Many workers anticipate noticeable changes as seasoned colleagues retire, but their responses also highlight clear opportunities for organizations to support smoother transitions. Workers shared where they expect pressures to increase and where additional planning could strengthen team readiness.
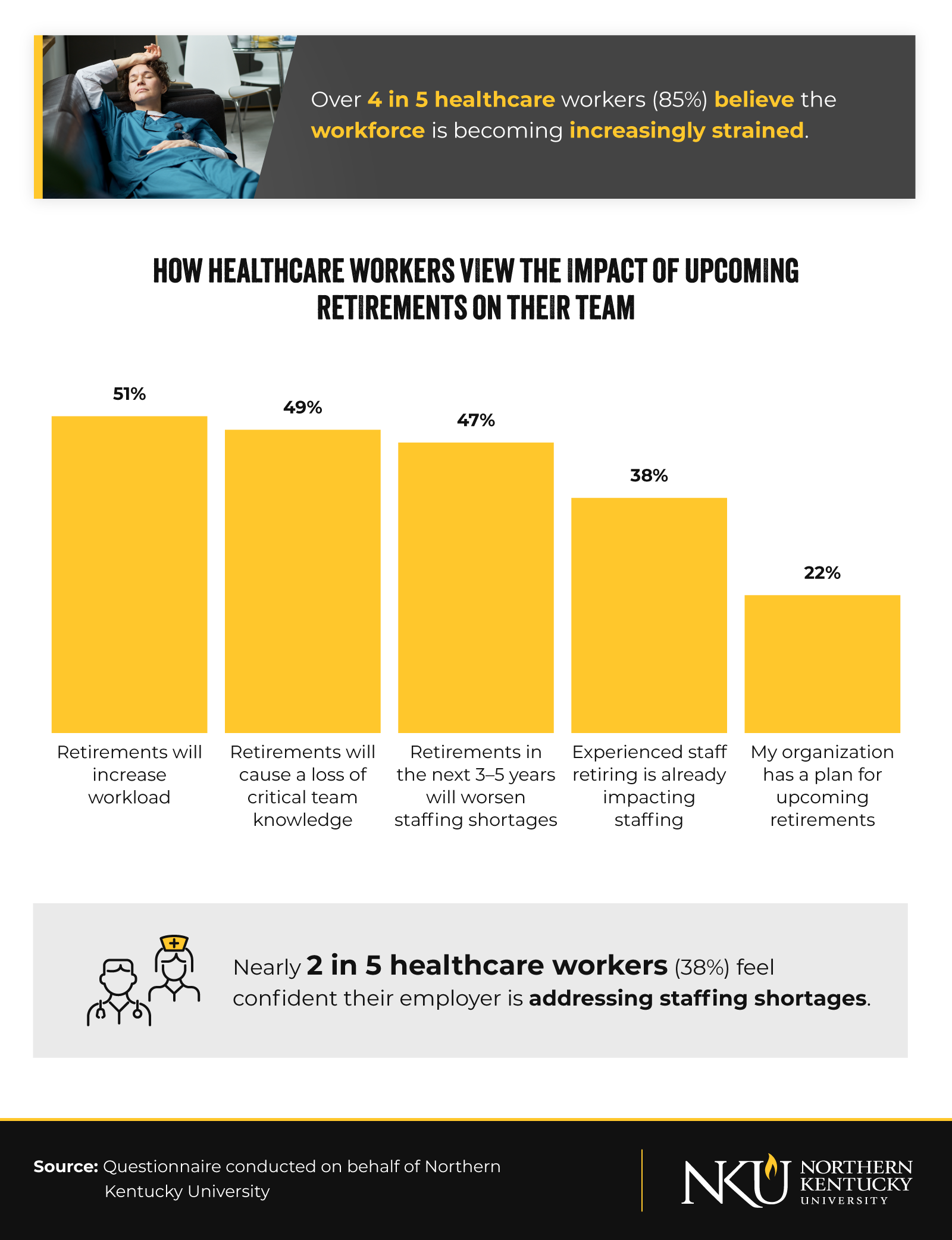
- Over half of healthcare workers (51%) believe that upcoming retirements will increase their workload, yet many already feel confident in adapting, with more than half (55%) believing they could reskill into a new role within six months if needed.
- Even as 85% say the workforce is growing more strained, 63% are interested in reskilling or upskilling in two years, signaling strong motivation to grow and stay in the field.
- About one in two healthcare workers (49%) would recommend a career in healthcare to someone entering the field today.
- One in three healthcare workers believe the next generation will have better working conditions than they do now.
- Nearly two in five workers (38%) feel confident their employer is addressing staffing shortages, showing early progress in workforce strategies that can be further strengthened.
Biggest Drivers of Healthcare Worker Workload
- 53%: Patient volume/acuity
- 49%: Documentation/administrative tasks
- 40%: Staffing shortages/last-minute coverage
- 22%: Training or onboarding new/float staff
- 20%: Regulatory reporting/quality metrics
- 19%: Care coordination across settings
- 19%: Prior authorizations/coordination with payers
- 12%: EHR usability issues
Main Barriers to Healthcare Worker Reskilling
- 48%: Tuition/cost
- 37%: No paid time to train
- 27%: Family or caregiving responsibilities
- 26%: Unclear career pathway
- 24%: Limited available training during preferred hours
- 24%: Unsure which skills will be most valuable
- 22%: Lack of employer sponsorship or support
- 17%: Shift coverage is unavailable
Technologies Expected to Reduce Workload in the Next 12 Months
- 33: AI documentation/ambient scribing
- 33: Automation of administrative tasks
- 24: Predictive staffing and scheduling tools
- 17: Virtual care/telehealth
- 16: Clinical decision support
Despite current and future pressures, many workers demonstrate adaptability. Their insights suggest that targeted planning, efficient workflows and stronger onboarding practices can help teams prepare for changing staffing patterns.
Career Sustainability, Training and Workforce Retention Outlook
Healthcare professionals also shared views about their long-term careers, opportunities to learn new skills and the factors influencing whether they remain with their employers. Their responses point to a workforce that, while navigating real challenges, maintains a strong commitment to the field.
- Nearly nine in 10 healthcare workers (86%) feel their job is secure over the next year.
- Just over half of healthcare workers (54%) believe their team has adequate staffing to provide high-quality care, and 52% say they feel burned out from their work.
Likelihood of Leaving Current Employer
- 23%: Likely to leave within the next 12 months
- 41%: Likely to leave within the next two to three years
- 53%: Likely to leave within the next five years
Retirement-related Issues Contributing to the Likelihood of Leaving
- 44%: Burnout related to ongoing turnover
- 35%: Concern that staffing shortages will worsen
- 22%: My organization’s lack of a clear plan for upcoming retirements
- 22%: Increased workload due to retirements
- 20%: Loss of experienced colleagues or institutional knowledge
Burnout from ongoing turnover disproportionately affects younger healthcare workers. Half of Gen Z (50%), 46% of millennials and 44% of Gen X staff cite it as a reason for considering leaving their employer, compared to just 31% of baby boomers.
Healthcare Workers Express Confidence in Career Longevity and Emerging Tools
- More than four in five healthcare workers (81%) expect to remain in the field for at least two more years, highlighting strong commitment and long-term engagement across the workforce.
- About one in three workers expect AI-driven documentation and administrative automation to reduce their workload in the year ahead, a promising sign that emerging tools may enhance sustainability.
- Two-thirds of healthcare workers (66%) feel their long-term career is personally sustainable, underscoring the field’s continued stability despite ongoing pressures.
Preparing for Change With Confidence and Adaptability
This research reveals a healthcare workforce balancing the realities of upcoming retirements with a forward-looking approach to career development and team sustainability. Workers acknowledge staffing pressures, yet many remain confident in their job security, motivated to learn new skills, and committed to the field. These perspectives point to practical opportunities for organizations to invest in training, strengthen planning efforts and build adaptable teams prepared for long-term success.
Methodology
This report is based on a national questionnaire of 300 healthcare workers across the U.S., conducted from December 1 to 3, 2025. The questionnaire set out to assess the readiness, pressures and priorities of today’s healthcare workforce as baby boomer retirements accelerate and staffing shortages intensify. Respondents were asked about job security, burnout, reskilling opportunities, retirement preparedness, organizational trust and the perceived impact of emerging technologies such as automation, AI documentation tools and virtual care.
While the findings offer a timely snapshot of frontline sentiment and provide valuable directional insight into the sustainability of the U.S. healthcare workforce, the sample size and self-reported nature of the data present limitations. Results should be interpreted as indicative rather than definitive, serving as a useful foundation for future research, workforce planning efforts and policy development.
About Northern Kentucky University
Northern Kentucky University offers flexible online programs that help working professionals advance their careers in healthcare. The online Master of Science in Healthcare Administration (MHA) program supports students in developing management and leadership skills that align with today’s evolving workforce needs.
Fair Use Statement
This information may be shared for noncommercial purposes with proper attribution. Please include a link to Northern Kentucky University when referencing or distributing this content.